An Online Survey of Technology Use Among Patients With Cancer Aged 65 Years or Older
Background: Historically, people aged 65 years or older have been slower to adopt new technology. However, technology use in this demographic continues to increase.
Objectives: This study aimed to understand how patients with cancer who are aged 65 years or older engage with technology and whether patient behavior related to technology use has changed because of the COVID-19 pandemic. In addition, this study evaluated whether respondents’ understanding of technology was associated with increased likelihood of adoption and perceived utility of the ONS On-Call™ cancer treatment symptom assessment tool.
Methods: A U.S. population–based anonymous online survey was conducted between May 17 and May 31, 2021, with 103 patients with cancer aged at least 65 years.
Findings: The majority of respondents used technology regularly as part of their daily lives. Activities included shopping online, reading the news, or engaging with a healthcare platform. As a result of the COVID-19 pandemic, most respondents reported an increased use of digital activities, particularly the use of healthcare technology. Respondents reported they would be likely to use ONS On-Call, particularly if it is recommended by a healthcare provider.
Jump to a section
Earn free contact hours: Click here to connect to the evaluation. Certified nurses can claim no more than 1 total ILNA point for this program. Up to 1 ILNA point may be applied to Professional Practice/Performance. See www.oncc.org for complete details on certification.
Technology use and adoption by people aged 65 years or older has been shown to be lower when compared to younger groups, and some individuals believe that this older adult population is less able to complete tasks necessary for use, such as two-factor authentication (Anderson & Perrin, 2017; Kakulla, 2021). Challenges such as costs, knowledge gaps, and privacy concerns can limit technology adoption and use by people aged 65 years or older (Anderson & Perrin, 2017; Kakulla, 2021). In an AARP survey, about half of older adults reported that they did not understand their electronic devices and would benefit from training on their use, with one-third of adults disclosing a lack of confidence in using technology (Kakulla, 2021).
Although there may be a digital divide between younger and older individuals, adults aged 65 years or older are increasingly adopting technology to obtain health information and better understand their health conditions (Bol et al., 2018; Hung et al., 2020). At least one-third of older adults report that they have and use smartphones or tablets, and many prefer tablets in a clinical setting to receive patient education (Anderson & Perrin, 2017; Bol et al., 2018; Kakulla, 2021; Ramprasad et al., 2019). Compared to individuals aged 80 years or older, those aged 65–79 years are twice as likely to use the internet and have broadband at home and are more than three times as likely to own a smartphone (Anderson & Perrin, 2017; Kakulla, 2021).
The COVID-19 pandemic resulted in a dramatic increase in technology use and adoption by people aged 65 years or older (Hasson et al., 2021; HealthInsurance.com, 2020; Kakulla, 2021). During the pandemic, patient isolation and access to care and treatment became major issues, particularly for older adults and patients with cancer (Haase et al., 2021; Nguyen et al., 2020; Verma et al., 2022). Healthcare providers and patients quickly became more comfortable using healthcare technology platforms to manage communication and care (Handley et al., 2021; Verma et al., 2022). Recommendations to improve care during the pandemic frequently included greater technology integration into care, increased telehealth utilization and availability, and support for patient use of technology (Haase et al., 2021; Verma et al., 2022).
According to Ramprasad et al. (2019), older adults prefer receiving information via tablets instead of verbal or paper information provided by a nurse. In an oncology setting, nurses provide guidance and education to patients. In fact, many older adults welcome the opportunity to communicate with their oncology care team from their home using health information technology, and nurses may be a primary point of contact (Hoogland et al., 2020). Many healthcare sites provide primarily telehealth-driven oncology clinics to offer continuity and increased touchpoints for patients prescribed oral oncolytics (Mathur et al., 2022).
The Oncology Nursing Society (ONS) has developed an oncology-specific decision support tool called ONS On-CallTM, which serves as a cancer treatment symptom assessment tool for oncology nurses. ONS On-Call includes a web-based survey designed to capture patients’ symptoms and guide standardized, evidence-based symptom assessment. The self-reported information feeds into the patient’s electronic health record, where oncology nurses can leverage ONS’s proprietary evidence-based resources to help guide and manage their patient’s care. For the purposes of this study, ONS On-Call was tested with potential patients from a desktop version, but its platform is applicable to mobile users as well.
This survey aimed to understand how patients with cancer who are aged 65 years or older engage with technology and whether patient behavior related to technology use has changed because of the COVID-19 pandemic. In addition, because more than half of all cancer cases are diagnosed among those aged 65 years or older (National Cancer Institute Surveillance, Epidemiology, and End Results Program, 2022), this survey evaluated whether respondents’ understanding of technology was associated with increased likelihood of adoption and perceived utility of the ONS On-Call cancer treatment assessment tool in this patient population.
Methods
Procedures
An anonymous, cross-sectional online survey of patients aged 65 years or older with a self-reported cancer diagnosis was conducted between May 17 and May 31, 2021. All respondents were recruited via email from two online survey panels to which respondents provided permission to be contacted for research purposes. Based on information in their databases, the panel companies emailed invitations to potential survey respondents who may meet the survey’s criteria.
Respondents qualified for the survey if they were a U.S. resident aged 65 years or older and were currently undergoing treatment for cancer, had completed cancer therapy within the past 24 months, or were undergoing hormone treatment as maintenance therapy. Respondents whose cancer treatment included surgery only and did not include therapeutic treatment or those who had received an organ transplantation as part of their cancer treatment were excluded. All respondents provided consent to participate and had the option to end their participation at any time. For completing the survey, respondents received modest monetary compensation.
Because the survey was conducted anonymously online as a market research study with no personally identifiable information collected and no intervention, the study was not submitted for review by an ethics committee. Researchers employed by ONS and KJT Group, Inc., a marketing firm, ensured that the survey was conducted in accordance with the principles and guidelines established by the Office for Human Research Protections and the Insights Association Code of Standards and Ethics.
The survey team conducted qualitative research to inform the design of the qualitative survey. Developed by ONS and KJT Group, Inc., the online survey consisted of a variety of binary, multiple-choice, Likert-type scale, and open-ended questions. The quantitative survey was not validated.
Statistical Analyses
Descriptive statistical analysis (means, frequencies) was performed using Q Research Software for Windows 23. Chi-square and t tests were also performed to evaluate differences within respondent types; additional analyses were performed using Stata/IC, version 14.1. Statistical significance was set at p < 0.05, using two-tailed tests. Data are presented as numbers and percentages for categorical variables, and continuous data are expressed as means and standard deviations unless otherwise specified.
Results
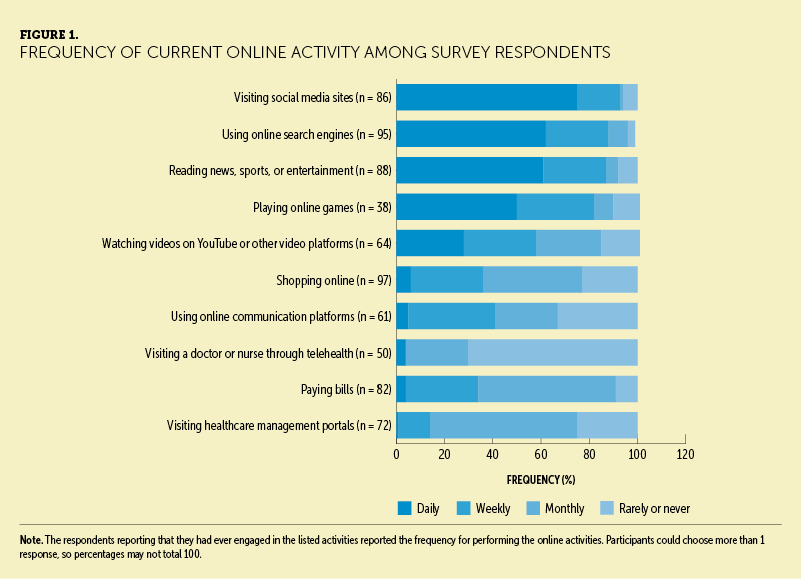
Sample Characteristics
Of the 1,243 respondents who entered the survey, 1,007 did not meet the eligibility criteria and 133 did not finish the survey. A total of 103 respondents completed the survey and were included in the results (see Table 1). The median survey length was 11 minutes. More than half (n = 58) of respondents were male, and the majority (n = 62) were aged 65–74 years. Fifty-six respondents reported an education level of a bachelor’s degree or higher.
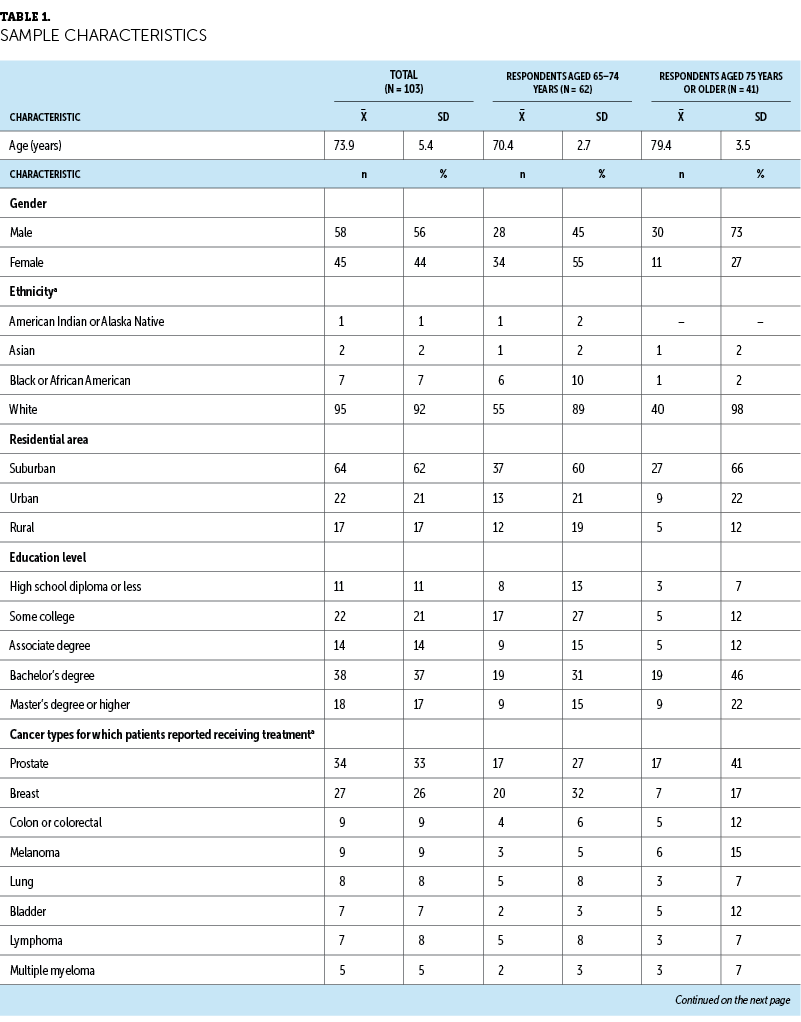
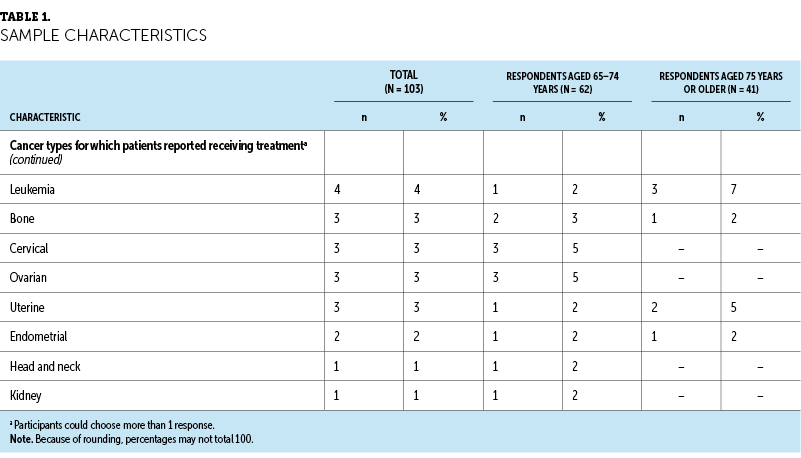
Half (n = 53, 51%) of respondents reported spending three or more hours per day on the internet on a computer, whereas only 20 (19%) reported spending three or more hours on the internet on a smartphone. These results were similar for respondents aged 65–74 years and respondents aged 75 years or older. Common activities included shopping online (n = 97); using online search engines (n = 95); reading news, sports, or entertainment (n = 88); and visiting healthcare management portals (n = 72). These results did not differ by age group. Among respondents who reported engaging in the listed activities, most reported daily use of social media and online search engines or reading online news. For most respondents, activities such as paying bills online and visiting healthcare portals often occurred monthly (see Figure 1).
To evaluate whether patient interactions with technology have changed as a result of the COVID-19 pandemic, respondents were asked how long ago they first performed specific activities. Among those who reported having performed online activities such as using search engines and reading news, sports, or entertainment, most were initiated more than three years ago (see Figure 2). For all activities, at least one-third of respondents engaged in the online activity for the first time in the past year. Of note, among those who have ever had a telehealth visit, almost three-fourths had their first telehealth visit in the past year.
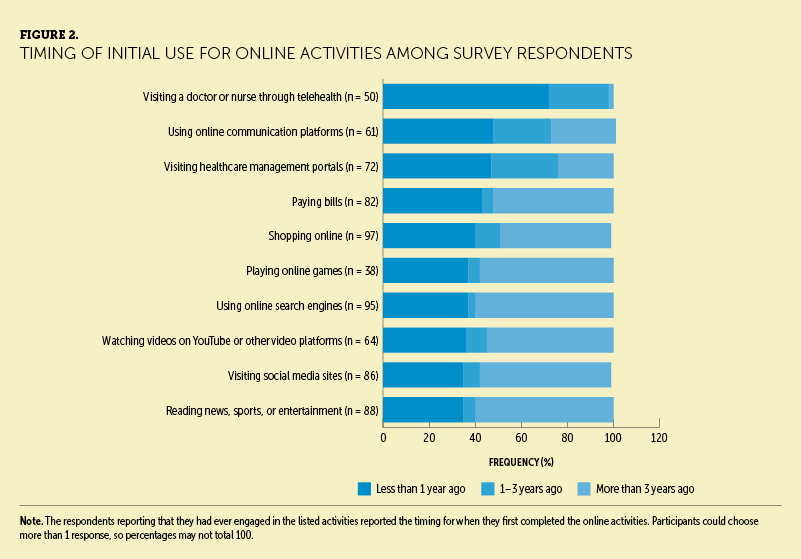
Within the past year, nearly half of respondents reported initiating using online communication platforms and visiting healthcare management portals. Among respondents who engaged in certain online activities every month, more than 50% of respondents reported that their online activity had not changed (range across eight activities = 34–92) because of the COVID-19 pandemic for most online activities, including visiting healthcare management portals and online communication platforms. Among those who used online communication platforms (n = 41) and telehealth (n = 15) at least monthly, the majority of respondents reported that their use of online communication platforms (n = 29, 71%) or visiting a doctor or nurse through telehealth (n = 10, 67%) increased in the past year.
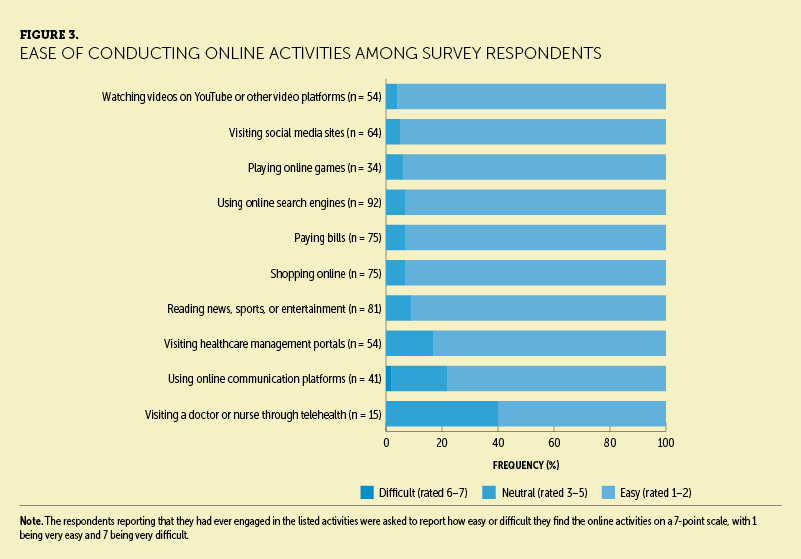
Among respondents who conducted certain online activities more than once per month, most reported finding those online activities easy, with few finding any online activity difficult (see Figure 3). Less than one-fourth of respondents reported that they needed a friend or family member to assist them with online activities in the past year. Survey results indicated that needing assistance was more common in respondents aged 75 years or older than in those aged 65–74 years. When assistance was needed, the most common activities included visiting a doctor or nurse through telehealth, shopping online, using online communication platforms, and visiting healthcare management portals.
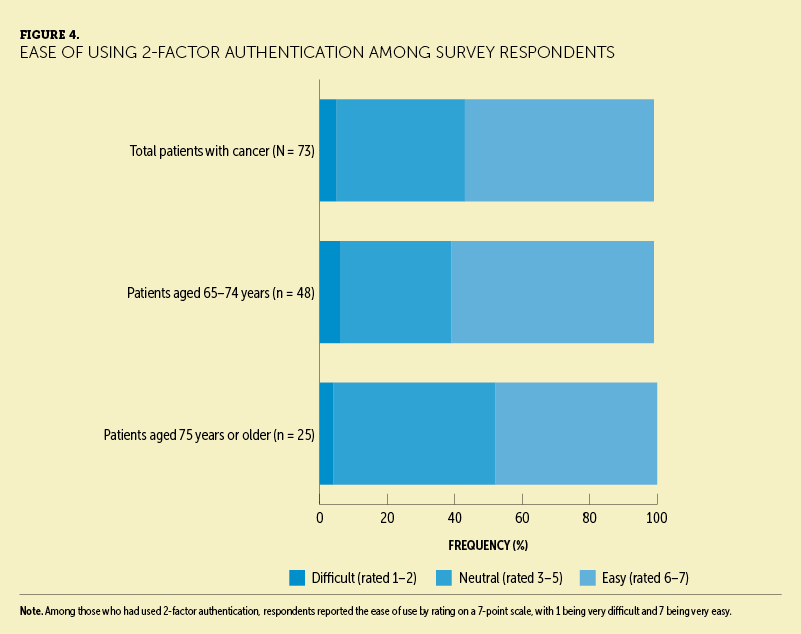
Nearly three-fourths (n = 73, 71%) of all respondents reported using two-factor authentication to log into a secure online website. This was more common in respondents aged 65–74 years than those aged 75 years or older (n = 47 [77%] versus n = 25 [61%], respectively). Among those who had used two-factor authentication (n = 73), 41 (56%) reported that using it was easy, which was more common in respondents aged 65–74 years (see Figure 4).
To understand whether survey respondents would be willing to engage with a symptom assessment tool, they were first asked to watch a brief video describing the tool. After watching the video, one-third (n = 35, 34%) of respondents reported they were likely to use ONS On-Call. When the use of ONS On-Call was recommended by a healthcare provider, respondents’ willingness to use the tool increased to 59%. For respondents aged 75 years or older, a recommendation from a healthcare provider increased respondents’ likelihood of using the tool from 27% to 61%. This increase was much greater than that for respondents aged 65–74 years, whose likelihood of using the tool increased from 39% to 58% following a healthcare provider’s recommendation.
Discussion
Results from this survey indicated that patients aged 65 years or older with cancer report that technology is an integral part of their lives. Survey respondents reported a substantial increase in use of healthcare technology in the past year, and the survey findings indicate that healthcare technology adoption may be generalizable to patients with cancer. The results of this survey align with other studies that support health-related technology adoption, and its use in older adult patients with cancer is increasing across a range of platforms. Although survey respondents aged 65–74 years reported that they were generally more comfortable with technology than those aged 75 years or older, the differences in responses between these groups were unremarkable, suggesting that individuals aged 65 years or older have broadly adopted technology use in their daily lives.
Although recommendations for including technology in clinical trial execution and general care for older populations emerged prior to COVID-19, they have become a key focus as a result of the pandemic (Hasson et al., 2021; Mannheim et al., 2019; Mitzner et al., 2018). Use of technology has been heavily influenced by the COVID-19 pandemic, and survey respondents reported a large increase in health-related technology use in the past year. Many used telehealth platforms for the first time as a result of the COVID-19 pandemic.
Technology adoption models have been shown to be different for people aged 65 years or older, and this can be considered when developing future tools and resources (Mitzner et al., 2018). However, it is largely believed that technology platforms will remain an integrated and long-term component of clinical trials and general healthcare management (Handley et al., 2021; Hasson et al., 2021).
In the current study, survey results indicated that healthcare provider recommendations substantially increased the likelihood of respondents using the symptom assessment tool. Further research to understand the factors that affected increased technology use during the COVID-19 pandemic are needed, particularly focused on what activities lead to adoption with high satisfaction; likelihood to continue utilization; and the extent to which a recommendation and use of technology by a patient’s medical team influences their adoption. Necessity and limited access to traditional care have been critical drivers during the COVID-19 pandemic. Determining which aspects of care are needed to maintain personal relationships with clinicians and care management of patients to positively affect psychosocial outcomes will be necessary in implementing future integrated digital healthcare platforms.
Limitations
There are several limitations to this study. Data were collected within a two-week period; thus, the respondent pool was limited to those who were willing and able to complete the survey during that time frame. The respondents to this survey may represent a group of people with higher education, skill, or comfort levels in engaging with online technology. Respondents may also have used technology in their careers and been more comfortable with using it. People without access to the internet were not included in the study. The authors did not seek out respondents with lower access to technology and recognize this as a limitation. Future studies could include strategies to engage people who may not regularly partake in online surveys or who are not regular users of the internet.
Survey respondents were recruited via email through an online panel company. Therefore, the results may not be generalizable to a population that is demographically different than the one sampled. Respondents had higher socioeconomic statuses and education and income levels, which are associated with better access to technology and health care (Anderson & Perrin, 2017; Harris et al., 2017; Vogels, 2021). In addition, respondents were predominantly White, and race has also been shown to influence technology access and literacy (Anderson & Perrin, 2017; Harris et al., 2017; Vogels, 2021).
Implications for Nursing
Results from this survey support that technology adoption and use are not limiting for older adult patient populations, particularly for web-based platforms similar to ONS On-Call. There was an increased likelihood of use of healthcare technology such as the ONS On-Call cancer treatment symptom assessment tool among patients aged 65 years or older, particularly when the tool was recommended by a healthcare provider. This survey’s results suggest that recommendations by healthcare providers, including nurses, may motivate patients to engage with and use technology. In addition, this survey’s results stressed the importance of tailoring interventions for the individual patient rather than for a given population. In addition to assessment of other age-related factors experienced by some patients in this population, nurses can evaluate older adult patients’ experience with technology. As this study illustrated, an increasing number of older adult patients are using technology on a routine basis. Nurses have a unique opportunity to assist patients’ use of technology with tools available to support their care, particularly in the complex setting of oncology.
Technology can serve as an important adjunct to the healthcare setting, and, when appropriately managed, digital platforms can provide a stronger sense of connectivity between patients and healthcare providers (Haase et al., 2021; Hasson et al., 2021; Sessa et al., 2022). Some forms of technology, such as tablets, have been shown to improve the way these patients communicate with their healthcare team (Hasson et al., 2021). Based on the results from this survey, ONS On-Call is one example of how integrated digital healthcare solutions may improve care for patients and overall healthcare providers, including nurses.
Conclusion
Results from this survey demonstrated that people with cancer aged 65 years or older are familiar and comfortable with using technology and web-based platforms in their daily lives. Based on survey responses, use of technology was heavily influenced by the COVID-19 pandemic, with respondents reporting an increase in the adoption of health-related technology in the past year to stay connected with healthcare providers and communicate with nurses. ONS On-Call may be a useful technology platform to improve the patient experience by allowing patient-provided information to reach oncology care teams. Development of health-related technology is likely to be adopted, particularly when the technology is recommended by a healthcare provider. Oncology nurses who use online surveys for patients may feel more comfortable recommending them to patients, knowing it will inform their care decisions.
About the Authors
Karen Hammelef, DNP, RN, CPM, is the director of products at the Oncology Nursing Society in Pittsburgh, PA; Keith Schoonover, MS, is the vice president of research and Paul Durlak, PhD, is a qualitative manager, both at KJT Group, Inc. in Rochester, NY; and Michele Galioto, DNP, RN, CNS, was, at the time of this writing, the executive director of the Center for Innovation at the Oncology Nursing Society. The authors take full responsibility for this content. This study was supported by the Oncology Nursing Society. Medical writing and editing support were provided by Elizabeth Tanner, PhD, and John Newman, PhD, of KJT Group, Inc., through funding from the Oncology Nursing Society. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Hammelef can be reached at khammelef@ons.org, with copy to CJONEditor@ons.org. (Submitted June 2022. Accepted November 16, 2022.)
References
Anderson, M., & Perrin, A. (2017). Tech adoption climbs among older adults. Pew Research Center. https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-am…
Bol, N., Smets, E.M.A., Burgers, J.A., Samii, S.M., De Haes, H., & Van Weert, J.C.M. (2018). Older patients’ recall of online cancer information: Do ability and motivation matter more than chronological age? Journal of Health Communication, 23(1), 9–19. https://doi.org/10.1080/10810730.2017.1394400
Haase, K.R., Kain, D., Merchant, S., Booth, C., Koven, R., Brundage, M., & Galica, J. (2021). Older survivors of cancer in the COVID-19 pandemic: Reflections and recommendations for future care. Journal of Geriatric Oncology, 12(3), 461–466. https://doi.org/10.1016/j.jgo.2020.11.009
Handley, N.R., Heyer, A., Granberg, R.E., Binder, A.F., Gentsch, A.T., Csik, V.P., . . . Rising, K.L. (2021). COVID-19 pandemic influence on medical oncology provider perceptions of telehealth video visits. JCO Oncology Practice, Op2100473. https://doi.org/10.1200/op.21.00473
Harris, C., Straker, L., & Pollock, C. (2017). A socioeconomic related ‘digital divide’ exists in how, not if, young people use computers. PLOS ONE, 12(3), e0175011. https://doi.org/10.1371/journal.pone.0175011
Hasson, S.P., Waissengrin, B., Shachar, E., Hodruj, M., Fayngor, R., Brezis, M., . . . Wolf, I. (2021). Rapid implementation of telemedicine curing the COVID-19 pandemic: Perspectives and preferences of patients with cancer. Oncologist, 26(4), e679–e685. https://doi.org/10.1002/onco.13676
HealthInsurance.com. (2020). Medicare eligible seniors survey findings: Technology, COVID-19, the 2020 election and more. https://www.healthinsurance.com/learning-center/article/medicare-eligib…
Hoogland, A.I., Mansfield, J., Lafranchise, E.A., Bulls, H.W., Johnstone, P.A., & Jim, H.S.L. (2020). eHealth literacy in older adults with cancer. Journal of Geriatric Oncology, 11(6), 1020–1022. https://doi.org/10.1016/j.jgo.2019.12.015
Hung, L.-Y., Lyons, J.G., & Wu, C.-H. (2020). Health information technology use among older adults in the United States, 2009–2018. Current Medical Research and Opinion, 36(5), 789–797.
Kakulla, B. (2021). Tech trends and the 50-plus: Top 10 biggest trends. AARP Research. https://doi.org/10.26419/res.00420.001
Mannheim, I., Schwartz, E., Xi, W., Buttigieg, S.C., McDonnell-Naughton, M., Wouters, E.J.M., & van Zaalen, Y. (2019). Inclusion of older adults in the research and design of digital technology. International Journal of Environmental Research and Public Health, 16(19), 3718. https://www.mdpi.com/1660-4601/16/19/3718
Mathur, A.D., Maiers, T.A., & Andrick, B.J. (2022). Impact of a pharmacist-led telehealth oral chemotherapy clinic. American Journal of Health-System Pharmacy. https://doi.org/10.1093/ajhp/zxac038
Mitzner, T.L., Savla, J., Boot, W.R., Sharit, J., Charness, N., Czaja, S.J., & Rogers, W.A. (2018). Technology adoption by older adults: Findings from the PRISM trial. Gerontologist, 59(1), 34–44. https://doi.org/10.1093/geront/gny113
National Cancer Institute Surveillance, Epidemiology, and End Results Program. (2022). Cancer stat facts: Cancer of any site. National Institutes of Health. https://seer.cancer.gov/statfacts/html/all.html
Nguyen, N.P., Vinh-Hung, V., Baumert, B.G., Zamagni, A., Arenas, M., Motta, M., . . . Thariat, J. (2020). Older cancer patients during the COVID-19 epidemic: Practice proposal of the International Geriatric Radiotherapy Group. Cancers, 12(5), 1287. https://www.mdpi.com/2072-6694/12/5/1287
Ramprasad, C., Tamariz, L., Garcia-Barcena, J., Nemeth, Z., & Palacio, A. (2019). The use of tablet technology by older adults in health care settings—Is it effective and satisfying? A systematic review and meta analysis. Clinical Gerontologist, 42(1), 17–26.
Sessa, C., Cortes, J., Conte, P., Cardoso, F., Choueiri, T., Dummer, R., . . . Tabernero, J. (2022). The impact of COVID-19 on cancer care and oncology clinical research: An expert’s perspective. ESMO Open, 7(1). https://doi.org/10.1016/j.esmoop.2021.100339
Verma, R., Kilgour, H.M., & Haase, K.R. (2022). The psychosocial impact of COVID-19 on older adults with cancer: A rapid review. Current Oncology, 29(2), 589–601. https://www.mdpi.com/1718-7729/29/2/53
Vogels, E.A. (2021). Digital divide persists even as Americans with lower incomes make gains in tech adoption. Pew Research Center. https://www.pewresearch.org/fact-tank/2021/06/22/digital-divide-persist…